In the jaws of sleep
The surprising relationship between insomnia and orthodontics; plus tips for better sleep and fan mail you shouldn't send to authors.
Hello there and happy Sunday,
Last week, I had an article come out in The Guardian about the medical gaslighting I experienced in my nearly four decade-long hunt for a solution to my chronic insomnia. Here’s an excerpt from that piece:
When I tell people that I have immense trouble with sleep, what they hear is that I’m difficult, neurotic, a diva with control issues. For nearly 40 years, every doctor I’ve pleaded with has announced that the problem is in my head. That I need to relax, take hot baths, do a lot of yoga. Or, you know, go back and be born a man, because ladies are high-strung.
But last year, at 45, I finally found a doctor who listened to my conviction that there was a physical root to my ailment.
This is the story of how I got through his office door.
You can read the rest of the article for free here, and I would love it if you did, because even if you don’t personally struggle with a sleep disorder, you might know someone who does and the information presented could help someone else or at least make them feel less alone.
On the topic of feeling less alone, I’ve been getting incredible responses to my article from fellow insomniacs and parents whose children have had orthodontic work and might be heading down the path of breathing and sleep issues that I travelled myself.
I’ve also received mail that made me want to set my hair on fire. In one such example, I received a one-thousand-word email from a male doctor writing to offer his condolences but also to suggest that the doctors who told me that my insomnia was in my head had not actually said that the problem was in my head; that perhaps I had not grasped the “medical parlance” of what was said to me by doctors. In other words, this male doctor decided that the best use of his time on a Thursday was to gaslight me about my experience with medical gaslighting.
I’m no stranger to upsetting communication from readers. No published author is. Usually I don’t respond to communications like this because engaging with these sorts of people creates more stress than the reception of the email or letter itself. But this mofo wrote me two days before I’m planning to march against the most repressive and patriarchal administration I’ve ever had the misfortune of trying to survive as a female artist under. It’s 2025 and I’m just not taking this bullshit anymore. I’m sharing my response to Mr. Medical Parlance, below.
A note before I do. Some of my friends—especially my women doctor friends—want me to name this man. I’m not going to do that. If I did, I can imagine he might be barraged with hate mail and I think someone with his psychological makeup would understand such backlash as proof of women’s “hysteria”; only convince him that he’s right. Whereas, if I keep his identity anonymous, inside the smaller space of our email exchange, Dr. Medical Parlance might actually learn something because his energy can (hopefully) be devoted to digesting what I’m saying, instead of parsing the ramifications to his career. Does that make sense? Anyway. Here is what I wrote back to this male doctor.
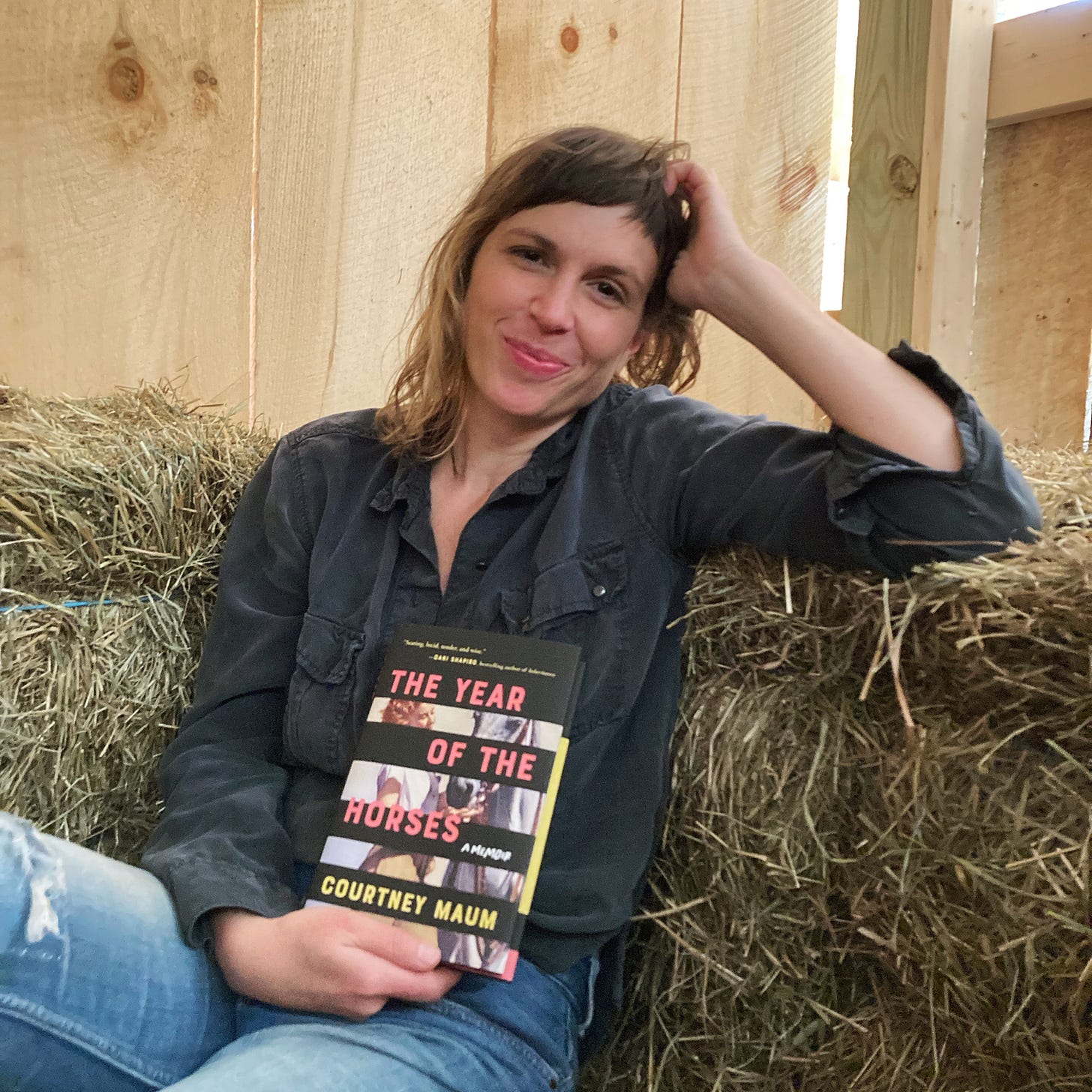
“I encourage you in this particular moment-- and especially in this particular cultural and political moment in the country I am writing from, the USA-- not to write the award-winning female author of 5 books who has published an article about being medically gaslit in a major publication that fact checks to inquire whether what she says was said to her was actually said. I have published a memoir about my experience (also fact checked) called The Year of the Horses in which I delve much further and deeper into my truly upsetting experiences with doctors, notably one with an anesthesiologist who punched me on the shoulder and said "don't worry, you'll make another one" right before preparing me for a D&C after a late term miscarriage. I made a formal complaint to the hospital in question on that occasion, but if I formally complained each time I was spoken to in an egregiously offensive manner by a doctor in my country (male, or female) it would be a full time job.
While I imagine that somewhere inside of you, your instincts to write me come from a good place, your instincts to question the veracity of what was medically said to me is totally misguided, not welcome and proof positive of the very issue I am writing about, which is specific to women's experience in doctor's offices, not men's. I have no need to continue this discussion further so please override your instincts to respond to this email-- I would prefer that you do not.
Thank you,
Courtney Maum
To date, Dr. Medical Parlance has not written me back. And I am proud of him for that.
Did you know that March was Sleep Awareness Month?
As I mentioned, readers have been sending me tons of recommendations for better sleep, so I wanted to share some of that advice in case it helps you or someone you love. I’m including bolded summaries of each suggestion so you can scan for what interests you. I’ve also edited out personal or identifying details to protect the commentators’ identity:
Disclaimer: I am not a doctor. I have not tried the methodologies and medications mentioned by readers below and I take no responsibility if you decide to try any of these methods yourself. I’m simply sharing selected recommendations in case they spark new ideas for people searching for better sleep.
Regarding CBT-I training and ACT instead: “I just came across your piece in The Guardian and just wanted to say that CBT-I can reinforce problems with insomnia because its tools (stimulus control, etc, i.e., control your thoughts and behaviour around something) are quite incompatible with the nature of sleep (a physiological process that can’t be controlled). ACT (Acceptance and Commitment Therapy) might be a better fit for this reason, and it’s helped lots of people, myself included (think letting go of the struggle, which is what’s keeping you awake, rather thank think your way out of it). I use Dr Guy Meadows’ Sleep School App and I recommend it :)”
Regarding GABA percentage in insomniacs/Camral: “Chronic insomniacs have on average a third less of the neurotransmitter GABA than people with good sleep health (this was the stuff I believe of a 2016 or so NIH study). It's the same with depressed people and certain neurotransmitters (I mean including probably that but more famously serotonin). But there are no approved meds that elevate GABA levels (without getting you high like hypnotics, benzos, and alcohol). [Redacted]….I started on the medication Campral, which is used to treat alcoholism (although more in Europe than in the US). It is thought to act on GABA, easing the anxiety that leads to relapse. My sleep, while still not perfect, is much better than it has been in decades.”
Myofunctional therapy: “I too, once suffered from small jaws. Along with growth appliances, my dentist had me see a Myofunctional Therapist. If you haven't tried this, it helps strengthen the tongue. The exercises makes the tongue leaner/stronger, so it stays in place better while sleeping. Many Drs, ENTs included, are unaware of this type of therapy. It's basically PT for your mouth and face.”
Autogenics: “Look into Autogenic Training! There are people in the US who offer it or there are online courses [through the] American Autogenics Society.”
Mirtazapine: “Just read your article on your insomnia. I was exhausted for decades. Four hours a night would have been an amazing blessing. Instead, I was lucky to get one or two. It was severely debilitating. No one got it. "Have you tried warm milk? Valerian?" A horse tranquilizer wouldn't put me down. I finally had an in-hospital sleep study. I thought I was up all night. I woke up over 40 times! The sleep specialist finally prescribed Mirtazapine. It has changed my life. I now sleep pretty much like a normal person. I don't wake up energized. But I am no longer barely coping. I've recommended it to several people. They've all been really grateful. Wishing you well, and a good night's sleep.”
Lighting solutions: “I just read your article, and while my sleep story isn’t like yours – it started at menopause, and I saw a six sleep specialists over the past 25 years - I recently figured out a non-pharmaceutical solution that is working. Philips Hue Natural Light Scenario: Wellbeing and circadian lighting These lights mimic the color temperature of sunlight across the day, getting yellower and then redder, and darker. Mine go on at 7 AM and are blue white, change a bit at 5 PM. At 8 PM, they become noticeably redder, and the room gets maybe 50% darker. At 10 PM, it gets another 50% darker and significantly redder. It’s too dark to read anything on paper – it’s kind of like well lit darkroom. My bedtime is midnight (I’ve trained myself to go to bed at midnight – I’m a night owl). Between 9 to 10 PM, I turn the screens on my Apple devices red, which completely blocks blue light, and stimulates melatonin.”

Thank you to those who continue to send me kind messages and helpful resources such as the ones above. A reminder that the full Guardian article about the relationship between sleep and orthodontics is here. And thank you, author Lara Prescott, poet Christina Stoddard and writer Sarah Canney for contributing to this piece!
Since I wrote the article, I have started CBT-I training with a real human. Fingers crossed that this leads me somewhere good! Wishing you good rest tonight and a nice end to your Sunday.
More soon,
Courtney
I write more about my experience with medical gaslighting, chronic insomnia and my fight for better physical and mental health in my memoir THE YEAR OF THE HORSES, available here or wherever books are sold. You’ll also learn outrageous factoids regarding the relationship between horses and humans, including the real reason for the invention of the side saddle.




I do not have long-term chronic insomnia (it sounds hellish, I truly cannot imagine) but I have had a few awful bouts of it since my mid-late 30s that are absolutely 100% hormonal - I still get regular periods, but perimenopause symptoms seem to start EARLY with the women in my family and last over a decade, and I have been determined to "get on it" aggressively and not suffer like my mother did. She basically didn't sleep, among other things.
Monkspepper, which naturally elevates progesterone, did wonders for me for a while. Since I started having very severe cyclical pain issues last fall (another fun bit of my matrilineal inheritance) I've switched to combined oral contraceptives, and I know that's not for everyone but honestly it's been a godsend, including for the creeping "brain fog" I've had in the last couple of years. That plus 5-htp supplements at night (which gently boost serotonin and melatonin) has me sleeping pretty well most of the time these days, as long as I'm keeping good routines overall. I'm assuming in a couple of years as my hormones continue to change, I'll have to adjust it all again.
Sorry to hear about the relapse. Great article. I’m sure it will help so many others. I only started having sleep issues during perimenopause and now menopause. I went to a naturopath who recommended a product called U Dream. It worked so well I thought it was a miracle. I joked with her “are you sure this is all natural? I think I could become addicted to this it works so well.” We laughed…fast forward a year or so later and there was a recall on the product because Lo and behold… they tested and found pharmaceuticals in it. So my instincts weren’t far off. Plus, the fact I’d go to the health food store and find women and men of all ages and stripes lining up to buy multiple packages when they got a shipment in was a giveaway something was up.
I kept some packages for a few years “just in case” I really needed a good nights sleep. I was that reluctant to part with my sure fire way to sleep—recall or no!
I can’t imagine living with that type of insomnia for decades. You are a warrior to have survived it!!